Dysphagia
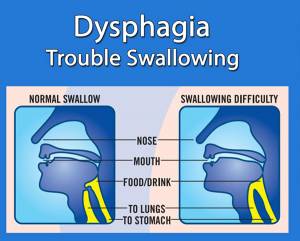 One of many potential complications of Myositis, including those with Dermatomyositis, Polymyositis, and Inclusion Body Myositis, is dysphagia, or trouble swallowing. Myositis can cause the throat muscles to weaken, thus making meal times difficult and sometimes dangerous.
One of many potential complications of Myositis, including those with Dermatomyositis, Polymyositis, and Inclusion Body Myositis, is dysphagia, or trouble swallowing. Myositis can cause the throat muscles to weaken, thus making meal times difficult and sometimes dangerous.
We should all be aware of what dysphagia is, learn about available treatments and procedures, and learn some tips that may provide help with swallowing food and liquids.
Dysphagia, can occur at any of the three stages in the swallowing process.
- Oral phase: Sucking, chewing and moving food/liquid into the throat
- Pharyngeal phase: Starting the swallowing reflex, squeezing food down the throat, and closing off the airway to prevent food or liquid from entering the airway (aspiration) or to prevent choking
- Esophageal phase: Relaxing and tightening of the openings at the top and bottom of the esophagus and squeezing food through the esophagus into the stomach
Symptoms of dysphagia can include inability to start the swallowing process, pain, an excessive amount of saliva, persistent coughing or choking while swallowing, frequent heartburn, overnight coughing, feeling like something is stuck in the throat or chest, weight loss, and dehydration due to lack of eating and drinking and taking much longer than normal to finish a meal. These symptoms can cause poor nutrition, risk of aspiration pneumonia, less enjoyment of mealtimes, and even embarrassment in social situations, which could lead to isolation and depression.
With myositis, muscles of the throat and upper airway may be affected, resulting in dysphagia, nasal regurgitation of fluids, aspiration, and hoarseness.
Tips to help during mealtimes
While the tips above may help, there is no better alternative than seeing a Speech-Language Pathologist.
Soft and Bite-Size Food Information Sheets
Check out the information sheets provided by The International Dysphagia Diet Standardisation Initiative (IDDSI).
Seeing a Speech-Language Pathologist for dysphagia
Speech-Language Pathologists (also called speech therapists) are trained in swallowing disorders and are able to diagnose dysphagia using a few methods.
First, they observe the patient to check for correct posture and oral movements during eating and drinking while also looking at the strength of the muscles involved in swallowing.
Speech-Language Pathologists may also order tests such as a modified barium swallow where the patient will eat or drink food that contains barium and then the swallowing process is viewed on X-ray. An endoscopic assessment (a lighted scope is inserted into the nose and then the swallow can be viewed on a screen) may also be ordered to help make a diagnosis and to prescribe treatment.
Once diagnosed with dysphagia, a Speech-Language Pathologist will create a treatment plan that will include helpful information such as exercises to help improve muscle movement, positions, and strategies to help make swallowing more safe and effective. Speech pathologists may also teach about specific food/liquid textures and consistencies to provide the patient with a diet for easier swallowing.
Some therapies for dysphagia
While these tips, exercises, and treatments may be helpful, it is also a good idea to learn the Heimlich maneuver and CPR. You can find classes in your area.
Find CPR ClassesAs a care partner, if you are not able to be home during mealtimes, some tips to make you feel comfortable may include:
Dysphagia-related studies and resources
Dysphagia Videos
Explanation of Dysphagia
Dysphagia & Thickened Liquids
Simply Put
“Simply Put” is a service of Myositis Support and Understanding, to provide overviews of Myositis-related medical and scientific information in understandable language.
MSU volunteers, who have no medical background, read and analyze often-complicated medical information and present it in more simplified terms so that readers have a starting point for further investigation and consultation with healthcare providers. The information provided is not meant to be medical advice of any type.