Myositis Autoantibodies
A diagnosis of one of the idiopathic inflammatory myopathies (IIM), or myositis, can be made through various methods including clinical and physical exam, thorough patient history, blood work, EMG, MRI, and often, a muscle or skin biopsy. When IIM is part of the differential diagnosis, Myositis-Specific Antibodies (MSA) should also be a part of the testing.
As the name suggests, the MSAs are specific to myositis. A physician can order the blood work for the MSA panel, however, if immune-mediated necrotizing myopathy (IMNM) is suspected the anti-HMGCR antibody must be ordered separately as it is not currently a part of the MSA panel.
Specific antibodies for Myositis patients
High-level overview of Myositis-Specific Autoantibodies
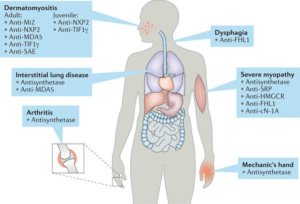
Studies show many myositis-specific autoantibodies (MSAs) that can be useful for the diagnosis as well as classification of the idiopathic inflammatory myopathies (IIM) because they have been shown to correlate with distinct clinical phenotypes.
Anti-Jo-1, anti-PL-7, anti-PL-12, anti-EJ, anti-KS, anti-OJ, anti-Ha, and anti-Zo antibodies target aminoacyl-tRNA synthetases and represent antisynthetase syndrome. Antisynthetase syndrome (AS) is characterized by myositis, interstitial lung disease, arthritis, fever, Raynaud’s phenomenon, and mechanic’s hands.
Anti-Mi-2, anti-MDA5 (anti-CADM140), anti-TIF1 (anti-155/140, anti-p155), anti-NXP-2 (anti-MJ), and anti-SAE antibodies are specific for dermatomyositis. In particular, anti-MDA5 antibodies are clinically associated with amyopathic dermatomyositis developing into rapidly progressive interstitial lung disease, whereas anti-TIF1 and anti-NXP-2 antibodies are closely correlated with cancer-associated dermatomyositis in adults. In addition, anti-TIF1 and anti-NXP-2 antibodies are predominant MSAs found in juvenile dermatomyositis, and the latter was correlated with a high incidence of calcinosis. Furthermore, anti-SRP and anti-3-hydroxy-3-methylglutaryl-coenzyme A (anti-HMG-CoA) antibodies have been found in patients with immune-mediatd necrotizing myopathy (IMNM).
Although the pathogenic role of MSAs remains unknown, recent studies have shown that myositis autoantigens are expressed at high levels in regenerating muscle fibers, which may initiate or amplify autoimmune responses in IIM.
Glossary of terms for autoantibody listing:
Below are abbreveiations used when discussing the autoantibodies.
- AS – Antisynthetase Syndrome
- PM – Polymyositis
- DM – Dermatomyositis
- JDM – Juvenile Dermatomyositis
- IBM – Inclusion Body Myositis
- IMNM – Immune-Mediated Necrotizing Myopathy
- ILD – Interstitial Lung Disease
- CAM – Cancer-Associated Myositis
- MCTD – Mixed Connective Tissue Disease
- RP – Raynaud’s Phenomenon
- RP-ILD – rapidly progressing interstitial lung disease
- SLE – Systemic Lupus Erythematosus
- Myositis* – May be PM or DM
- SS-A – Sjogren’s syndrome A
- SSc – Systemic Sclerosis or Scleroderma
- MDA5 – Melanoma differentiation-associated gene 5
- > – more often than
Myositis-Specific Antibodies (MSA)
MSAs can assist your doctor in helping to confirm a diagnosis of certain types of myositis such as polymyositis and dermatomyositis. They are also helpful in diagnosing Antisynthetase syndrome. These antibodies also offer some insight into potential complications you may experience during the course of your disease and potential treatment options that may work best.
It is estimated that 50% of patients with polymyositis or dermatomyositis have myositis-specific antibodies, so when a clinical exam and other testing suggest the possibility of myositis, the presence of these antibodies can be supporting evidence for a diagnosis. Myositis-specific antibodies have also improved our understanding of myositis by leading to the identification of certain clinical patterns.
Antisynthetase autoantibodies
ARS (aminoacyl transfer RNA (tRNA)) are a group of autoantibodies known as the antisynthetase autoantibodies. Eight (8) has been discovered thus far.
Anti-Jo1 (Histidyl-tRNA synthetase)
- PM, DM + ILD; Arthritis (75%), Raynaud’s Phenomenon (50%), Mechanics Hands (20%)
- Detected in 15-25% of patients with polymyositis/dermatomyositis (PM/DM)
- Most frequent tested of the ARS autoantibodies and the only one associated with classification criteria.
- Seasonal Onset Potentially: Spring
Anti-PL-7 (Threonly-tRNA synthetase)
- PM, DM + ILD; infrequent muscle involvement (hypomyopathic), severe arthritis
Anti-PL-12 (Alanyl-tRNA synthetase)
- ILD more often than myositis, pulmonary hypertension, esophageal involvement.
- Maybe just present as ILD.
Anti-EJ (Glycyl-tRNA synthetase)
- PM more often than DM + ILD
Anti-OJ (Isoleucyl-tRNA)
- ILD + PM/DM
Anti-KS (Asparaginyl-Transfer RNA Synthetase)
- ILD more often than myositis*
Anti-Zo (Phenylalanyl-tRNA synthetase)
- ILD + myositis*
Anti-YRS/HA (Tyrosyl-tRNA synthetase)
- myositis
Non-synthetase Autoantibodies
Anti-NXP-2 (Nuclear matrix protein 2)
- Associated with subcutaneous edema, calcinosis, and a severe muscle phenotype characterized by myalgia, proximal and distal weakness, and dysphagia.
- Increased risk of cancer, suggested they undergo comprehensive cancer screening
- Calcinosis is more frequent in younger patients and cancer more common in the elderly
- In JDM: Severe muscle atrophy and functional impairment
- associated with severe juvenile DM complicated by calcinosis, polyarthritis and intestinal vasculitis
Anti-Mi-2 (DNA helicase)
- DM with rash more often than muscle symptoms (clinically amyopathic dermatomyositis)
- Muscle biopsy may show prominent necrosis.
- First autoantibody recognized as specific for DM.
- Despite high CK levels, muscle involvement is often mild.
- Patients often respond well to corticosteroids.
- Based on the 2019 longitudinal cohort study, those with anti-Mi2-positive DM have more severe muscle disease than patients with anti-Mi2-negative DM or patients with AS. Anti-Mi2 autoantibody levels correlate with disease severity and may normalize in patients who enter remission. Muscle biopsy shows prominent necrosis.
Anti-HMGCR (anti 200/100)
- One of two known autoantibodies to diagnose IMNM.
- It can be statin-associated but even those who have never taken statin drugs may test positive.
- Anti-HMGCR Myopathy: Severe muscle weakness, highly elevated CK levels. Often resistant to available off-label medications.
Anti-MDA5 (anti-CADM 140)
Melanoma Differentiation-Associated gene 5 (MDA5)
- DM or CADM with interstitial lung disease (ILD), some with rapidly progressing ILD.
- Anti-MDA5 autoantibodies titer seems to correlate with disease activity and response to therapy
Anti-TIF1γ/α (anti-p155/p140)
- CAM in adults
- Widespread skin involvement is associated with unique features, such as palmar hyper-keratotic papules, psoriatic-like dermatitis and atrophic hypo-pigmented patches with telangiectasias.
- Clinically, two age group associations:
- younger than 40-year-old patients, with a classical DM at presentation
- older than 40-year-old patients, with cancer-associated myositis
- Two (2) antibodies directed against a 155 and 140 kDa, rapidly identified as TIF-1γ (TRIM33) and TIF-1α (TRIM24), respectively, and a third 120 kDa band, partially overlapping with anti-PL-12, identified as TIF1β (TRIM28).
- JDM
Anti-TIF1β
- Marker for DM
Anti-SAE (Anti-Sumo)
- Marker for DM
- Skin disease is often severe followed by muscle weakness.
- ILD seems to be rare, but severe dysphagia and systemic symptoms have been reported.
- Very few case reports to draw from.
Immune-Mediated Necrotizing Myopathy (IMNM) Autoantibodies
There are now two autoantibodies found to be associated with IMNM, sometimes called necrotizing autoimmune myopathy (NAM).
Anti-SRP (SRP – signal recognition particle)
This is often misdiagnosed as polymyositis.
- Severe, acute, and resistant immune-mediated necrotizing myopathy.
- One of two known autoantibodies to diagnose IMNM.
- Anti-SRP Myopathy: Severe weakness and functional disability
- Seasonal onset shown in studies: August and January
- Highly elevated CK levels. Often resistant to available off-label medications.
Anti-HMGCR (anti 200/100)
- One of two known autoantibodies to diagnose IMNM.
- IMNM with or without history of statin exposure
- Anti-HMGCR Myopathy: Severe muscle weakness, highly elevated CK levels. Often resistant to available off-label medications.
Learn more about IMNM
Learn more about IMNMNew Research as of Sep. 17, 2019
A new novel autoantigen, eukaryotic initiation factor 3 (eIF3), detected in idiopathic inflammatory myositis.
Identification of a novel autoantigen eukaryotic initiation factor 3 associated with polymyositis – Finding needs further confirmation, but it appears this is associated with polymyositis. Read the full article using the citation below.
Zoe Betteridge, Hector Chinoy, Jiri Vencovsky, John Winer, Kiran Putchakayala, Pauline Ho, Ingrid Lundberg, Katalin Danko, Robert Cooper, Neil McHugh, Identification of a novel autoantigen eukaryotic initiation factor 3 associated with polymyositis, Rheumatology, , kez406, https://doi.org/10.1093/rheumatology/kez406
Myositis-Associated Autoantibodies (MAA)
Below is a listing of some of the known Myositis-Associated Antibodies (MAA). These can be found in those with myositis as well as with other autoimmune diseases such as Lupus, Scleroderma, and overlapping conditions with myositis. As more research is completed and released we will know and share more.
- Anti-PM-Scl
- PM and SSc Overlap
- Anti-RNP (Anti-U1-snRNP)
- Anti-U1-snRNP is most commonly tested in clinical practice.
- High-titre anti-U1-snRNP targeting the 70kD protein are considered specific markers of mixed connective tissue disease (MTCD)
- Anti-U2-RNP, U5-RNP, and anti-U4/U6-RNP are also described in patients with PM/SSc overlap syndrome
- MCTD, overlap syndrome
- See citation below for the myositis clinical phenotype information.
- Anti-Ku
- Myositis* / SSc
- PM/SSc overlap syndromes and SLE, associated with arthralgia, Raynaud’s phenomenon and ILD
- Potentially severe, steroid-resistant ILD
- Anti-Ro52
- Myositis often with SS or SLE, with ILD
- Often coupled with other MSAs.
- Anti-Ro52 can be found in IIMs and are often associated with other MSAs, in particular anti-synthetase, anti-MDA5 and anti-SRP autoantibodies.
- Anti-Ro60/SSA
- SjS, SLE
- Anti-56 kDa
- Myositis, often with Jo-1
- Anti-KJ
- PM, ILD, RP
- Anti-synthetase-like syndrome
- Anti-Fer
- Anti-synthetase-like syndrome
- Anti-Mas
- Myositis, rhabdomyolysis, chronic hepatitis
- Myositis, rhabdomyolysis, chronic hepatitis
Anti-U1RNP – anti-U1-ribonucleoprotein (RNP) autoantibodies.
Based on 2018 longitudual cohort study, patients with anti-U1-RNP myositis typically present with proximal weakness and necrotizing muscle biopsies. Arthritis, dermatitis, and ILD are the most common extramuscular clinical features. Pericarditis and glomerulonephritis are uniquely found in patients with anti-U1-RNP–positive myositis.
Other Myositis associated antibodies
- Anti-AMA
- Anti-mitochondrial antibodies, may have cardiac involvement
- Anti-NT5C1A (anti-Mup44)
- Sporadic Inclusion Body Myositis
AMA Associated Myositis, Cardiac Involvement
Patients with inflammatory myopathy associated with antimitochondrial M2 antibodies (AMA) may have cardiac involvement, dropped head, and muscle atrophy. These antibodies bind to a protein in the mitochondria, the energy-producing factory of the cell. This may also be called “AMA-associated myositis.”
Heart disease may appear in the form of myocarditis (inflammation of the heart), severe arrhythmias, or cardiomyopathy (enlargement of the heart). Although the heart disease was often not recognized to be related to the myositis, treatments that suppressed the immune system led to improvements in these symptoms.
Anti-mitochondrial antibodies identify a distinct inflammatory myopathy phenotype that is frequently associated with chronic skeletal muscle disease and severe cardiac involvement. Diagnosing this early is essential for treatment.
Inclusion Body Myositis Antibodies
It has been recently discovered that some inclusion body myositis (IBM) patients may have antibodies that can help in making a correct diagnosis, along with additional testing. These antibodies are anti-cytosolic 5’ –nucleotidase 1A (anti-CN1A or anti-NT5C1A).
This autoantibody is positive in about one-half of IBM patients. A negative test does not mean a patient does not have IBM, however, a positive test makes it likely that inclusion body myositis is the correct diagnosis.
Polymyositis and Inclusion Body Myositis can appear much the same, especially at first. The NT5C1A antibody test can now help to distinguish the two as this antibody is rarely positive for those with polymyositis.
This antibody test is sometimes positive for other autoimmune diseases and is not stricly specific to IBM.
Autoantibodies for Myositis are currently undergoing more research:
Disclaimer: Research is ongoing on many of the autoantibodies listed on this page. Please note that as research continues and new evidence is found, we will try to keep this page updated. This is for informational purposes only based on information we have at the time of this writing.
Simply Put
“Simply Put” is a service of Myositis Support and Understanding, to provide overviews of Myositis-related medical and scientific information in understandable language.
MSU volunteers, who have no medical background, read and analyze often-complicated medical information and present it in more simplified terms so that readers have a starting point for further investigation and consultation with healthcare providers. The information provided is not meant to be medical advice of any type.