Dermatomyositis (DM)
Dermatomyositis is one of a group of rare muscle diseases called inflammatory myopathies, which are characterized by chronic muscle inflammation accompanied by muscle weakness. An identifying factor for dermatomyositis is a skin rash that precedes or accompanies progressive muscle weakness.
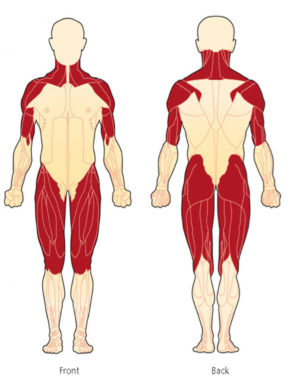
Muscle weakness, when present, can develop over a period of days, weeks, or months. This weakness often leads to difficulty climbing stairs, rising from a chair or from the floor, turning in bed, lifting, combing hair, or reaching over the head for something like an item on a shelf. Muscle weakness is typically symmetrical (same on both sides) and affects the proximal muscles (muscles closest to the body’s core) such as the hips, thighs, upper arms, shoulders, and neck.
A skin rash that precedes or accompanies muscle weakness is often helpful in diagnosing DM and maybe the first sign of the disease. People with darker skin may not notice the rash as readily. Muscle involvement, for some, is not a part of their disease.
Muscle pain (myalgia) and joint pain, with or without true arthritis and joint inflammation, can also be a part of dermatomyositis.
DM is a chronic, incurable disease.
Signs and Symptoms of Dermatomyositis
Not all patients display all of these symptoms.
- Skin rashes and discolorations which affect sun-exposed areas, cheeks, nose, shoulders, upper chest, and elbows.
- Proximal muscle weakness (muscles closest to the trunk, such as shoulders, thighs, and hips)
- Symmetrical muscle weakness (the same muscles on both sides of the body)
- Gottron’s papules or Gottron’s sign (bumps found over the knuckles, elbows, and knees, often with a raised, scaly break-out)
- Itching and changes in the scalp resembling psoriasis and hair loss
- Ragged cuticles, prominent blood vessels on the nail folds, and other nail-bed abnormalities
- Nonerosive inflammatory polyarthritis
- Joint inflammation
- Dry, scaly, or rough skin
- Fatigue (may be life-altering and disturb sleep patterns)
- Weight loss
- Low-grade fever
- Muscle pain (myalgia)
Other symptoms and complications
Each patient varies in symptoms/complications.
- Risk of falls due to muscle weakness
- Lung problems such as Interstitial Lung Disease (ILD), Pulmonary Fibrosis, or Labored breathing (dyspnea)
- Difficulty swallowing (dysphagia)
- Stomach (gastrointestinal) ulcers and intestinal perforations, also more common in children
- Calcinosis (hard, often painful lumps or sheets of calcium that form under the skin’s surface)
- Raynaud’s phenomenon
- A hoarse or changing voice (dysphonia)
- Inflammation of the fat which can feel like little bumps lying just under the skin and can be tender to the touch (panniculitis)
- Irregular heartbeat (arrhythmia)
- Inflammation of areas in the heart, myocardium or inflammatory cardiomyopathy
- Other connective tissue diseases (overlaps)
- Cardiovascular disease
- Complications and side effects related to treatment
- Increased risk of having certain types of cancer
- Aspiration pneumonia
Who is affected by Dermatomyositis?
Dermatomyositis is a rare disease. A rare disease in the U.S. is defined as a condition affecting fewer than 200,000 people.
Here is some additional information:
- DM affects twice as many women as men.
- DM is more common in African Americans, who, according to some studies, are affected at three-times the rate of the Caucasian population in the U.S.
- DM typically affects adults between 40-60 years old and children ages 5-15 and as young as 2 years old (Juvenile Dermatomyositis).
Antisynthetase Syndrome (ASyS)
Approximately 90% of those diagnosed with Antisynthetase syndrome experience a form of myositis, either polymyositis or dermatomyositis. This complex syndrome also includes interstitial lung disease (ILD), Raynaud’s phenomenon, inflammatory polyarthritis, mechanic’s hands, and fever.
Mixed Connective Tissue Disease (MCTD)
Mixed connective tissue disease is a rare autoimmune disease considered an “overlap” of three diseases; Systemic Lupus Erythematosus, Scleroderma, and Polymyositis.
Overlap Syndrome
Overlap Syndrome means having more than one autoimmune disease at the same time. This can include many diseases such as Lupus, Dermatomyositis, Polymyositis, Scleroderma, Raynaud’s phenomenon, and Sjögren’s syndrome.
Cancer and Dermatomyositis
About one-third of DM patients develop malignancy, often within 5 years before or after disease onset; breast and ovarian cancers in women, and lung and prostate cancer in men.
Other less frequently reported cancers include colorectal cancer, non-Hodgkin lymphoma, pancreatic, gastric and bladder cancer.
Cancer can be an underlying cause of dermatomyositis and may precede its onset. If cancer precipitated DM, removal of the cancer may result in remission of dermatomyositis.
Dermatomyositis in adults has also been linked to an increased likelihood of developing cancer post-diagnosis, particularly cancers of the cervix, lungs, pancreas, colorectal system, breasts, ovaries and gastrointestinal tract and non-Hodgkin’s lymphoma. The risk of cancer appears to level off about five years after onset of DM. The incidence of cancer is higher in dermatomyositis than in polymyositis, and particularly in those with certain antibodies. It is strongly suggested that appropriate cancer screenings be conducted upon diagnosis and in the years after a myositis diagnosis.
Because of a high cancer risk, both before and after diagnosis, doctors will often perform cancer screenings at the onset or suspicion of dermatomyositis. Cancer will continue to be a risk with such patients, and cancer screening should be continued on a regular basis and more often than suggested for the patient’s age group per doctor’s advice, particularly because of the increased cancer risk with immunosuppressive treatments.
Pain and Dermatomyositis
Muscle pain is a reality for many dermatomyositis patients, as are uncomfortable-to-painful and itchy skin rashes, ulcers, and for some, calcinosis.
Studies and reports do not say how many experience muscle pain, but an estimate based on information we received from an expert in the field, who sees a large number of patients in a myositis center, reported 50% of patients in her practice experience muscle pain.
After continuing to hear patients report their doctors saying “there is no pain with myositis” and based on personal experiences with the misapplied 2016 CDC Opioid guidelines, we surveyed the community. This pain survey was eye-opening, even to us, to finally have data showing that pain is a symptom for many of us, and even among the different types of myositis. Thanks to the MSU Research Team, the paper was submitted for publication in a prominent rheumatology journal and is being presented at several international conferences. You are not alone in the pain.
Dermatomyositis Education Sessions
with Dr. Victoria Werth
Characteristics of Dermatomyositis
Not everyone diagnosed with dermatomyositis will display all or even the same symptoms, and the intensity of the symptoms can vary.
Muscle Involvement
DM causes inflammation of the skeletal muscles, those involved with voluntary movement. Muscle weakness is symmetrical (same on both sides) and affects the proximal muscles (muscles closest to the body’s core) such as the hips, thighs, upper arms, shoulders, and neck.
In some cases, the distal muscles (those further away from the chest and abdomen such as the lower arms, hands, lower legs, and feet) may also be affected.
Muscle weakness can develop over a period of days, weeks, or months. This weakness often leads to difficulty climbing stairs, rising from a chair or from the floor, turning in bed, lifting, combing hair, brushing teeth, or reaching over the head for something like an item on a shelf.
Skin Involvement
One of the main signs and symptoms of DM, and the reason the term “dermato” is used, is skin involvement.
DM may be easier to diagnose compared to other forms of Myositis when patients present with typical skin findings such as Gottron’s Papules, Gottron’s Sign, and the heliotrope rash covering the eyelids and extending onto the face.
Skin rashes often appear on the eyelids and the face, as well as around the knuckles, nails, knees, elbows, upper back and shoulders (Shawl sign) and chest region (V-sign). Some rashes may be painful, severely itchy (pruritis), and intense enough to disturb sleep.
Scalp inflammation and thinning of the hair is also common.
In rare cases, cutaneous vasculitis, ulcerations, and calcinosis are observed, although more so with juvenile dermatomyositis.
Some commonly used terms:
- Heliotrope refers to the pink-purple-violet shade of the heliotrope flower.
- Violaceous Erythema refers to a violet color rash, often in patches, as a result of injury, irritation, or inflammation causing dilation of the blood capillaries.
- Macular Rash is characterized by a flat red area on the skin that is covered with small confluent bumps (merged together) that may go unnoticed in those with darker skin tones.
- Papules refer to small, raised, solid pimples or swelling, often forming part of a rash on the skin and typically inflamed, but does not produce pus.
Specific Skin Findings of DM
The appearance of some skin findings are “pathognomonic” for DM, meaning they are specific to the disease and can help make or confirm a diagnosis. These skin findings can cause major cosmetic issues and are often very itchy.
- Gottron’s Papules: Red, often scaly, bumps overlying the knuckles of the fingers, hands, elbows, or knees. Occurs in an estimated 70% of patients.
- Gottron’s Sign: Flat red rash over the back of the fingers, elbows, or knees.
Characteristic and Secondary Skin Findings of DM
- Shawl Sign: Widespread, flat, reddened rash across the shoulders and upper back, and can extend onto the back of the upper arms and up into the neck and scalp. Pattern of where a shawl would lay if wearing one.
- V-Sign: Widespread, flat, reddened rash covering the chest area, such as where the exposed skin would be when wearing a V-neck shirt.
- Heliotrope Rash: Violaceous (violet or purple) to dusky (can appear as lighter pink, especially in lighter-skin patients) rash over the eyelids, with or without swelling, in a symmetrical (both sides) distribution. In DM, this rash includes, or hugs, the nasolabial folds (laugh lines) unlike with similar rashes found with Lupus that spare this area.
- Samitz’s Sign: Cuticles can become red and ragged and can be painful. Cuticle overgrowth is also seen in some patients.
- Periungual Telangiectasia: Dilated blood vessels near the nails and under the fingernail.
- Mechanic’s hands: Roughening and cracking of the skin of the tips and sides of the fingers resulting in irregular, dirty-appearing lines that resemble those of a manual laborer.
- Photodistributed Violaceous Erythema: Violet color rash covering the sun-exposed areas such as the face and scalp. This finding shows that the sun can trigger and exacerbate DM/CADM.
- Poikiloderma: A secondary skin finding that includes pigmentary changes, skin atrophy, and telangiectasia (dilated vessels). This is very common with DM/CADM.
- Calcinosis: Often-painful lumps of calcium that can occur in the skin, muscle, and other connective tissues. This is found more with children and adults diagnosed with Juvenile Dermatomyositis (JDM). Surgical intervention may be required for some with severe and painful calcinosis.
- Plugging of the vessels may lead to skin blisters and skin ulcers.
- Scalp Inflammation with thinning of the hair and which may resemble psoriasis.
Dermatomyositis is a chronic disease with no cure, however, many people respond well to certain treatments or combination of treatments with improvement in skin and muscle symptoms or even complete remission.
Clinically Amyopathic Dermatomyositis (CADM)
There is a subset of DM which includes skin manifestations of DM with little-to-no muscle involvement. These include Amyopathic dermatomyositis (ADM) and Hypomyopathic dermatomyositis, together called Clinically Amyopathic Dermatomyositis (CADM). This is often referred to as dermatomyositis siné myositis, and skin-predominant dermatomyositis.
Some of the skin findings that suggest dermatomyositis include a violet-red-pink rash on the face, neck, forearms and upper chest; Gottron’s papules, Gottron’s sign, and heliotrope eyelids. Pruritus and photosensitivity are common, as is scalp inflammation and thinning of the hair.
Amyopathic Dermatomyositis (ADM)
While patients with amyopathic dermatomyositis usually do not have clinically evident muscle weakness or muscle findings.
Hypomyopathic dermatomyositis
Hypomyopathic DM includes a small amount of muscle involvement, which may not appear on the exam but is documented on diagnostic testing such as muscle enzymes.
Some cases of CADM have been associated with internal malignancy and/or interstitial lung disease and there is a higher risk for rapidly-progressing interstitial lung disease (ILD).
Treatment for CADM may include sun avoidance, ample use of sunscreen, topical steroids, antimalarial agents, immunosuppressive medications, intravenous (IV) immunoglobulin, and monoclonal antibody therapy (rituximab).
Diagnosing Dermatomyositis
Which doctors do I see?
Dermatomyositis is diagnosed and managed by a rheumatologist, dermatologist, or neurologist (neuromuscular), usually in coordination with a primary care physician (PCP). Consultation with other specialists may be required depending on your symptoms, other coexisting illnesses, and other organ involvement and may include a cardiologist, pulmonologist, oncologist, gastroenterologist, and pain management.
There are doctors trained in both dermatology and rheumatology which can be especially helpful for those with dermatomyositis. See Rheumatologic Dermatology Society (RDS).
Exercise is important for myositis patients. Therefore, you may also see a physical therapist, occupational therapist, and, if you have trouble swallowing (dysphagia), you may also see a speech-language pathologist.
Clinical and Physical Exam
A complete medical and family history is important in helping to diagnosis a rare and complex disease such as dermatomyositis. We suggest writing a detailed medical and family history that you can share with your medical team and that can be used for all future appointments.
Skin findings with DM can resemble Lupus SLE and are identical on a skin biopsy. An experienced dermatologist can use the skin exam to help better differentiate Lupus from DM.
Blood Testing
Your doctor will likely order various blood tests when suspecting dermatomyositis in order to measure autoimmune, inflammatory, and cancer markers and to check for Myositis-Specific and Myositis-Associated antibodies, and other antibodies. Some of these tests may include:
- Creatine Kinase (CK or CPK) (muscle enzymes)
- Aldolase
- ALT and AST
- LD (Lactate dehydrogenase)
- Sed Rate (also called ESR or Erythrocyte sedimentation rate)
- ANA (Antinuclear Antibodies panel)
EMG and Nerve Conduction Study (NCS)
An EMG (Electromyography) is a test that checks the health of the muscles and the nerves that control the muscles. With dermatomyositis, the EMG may show myopathic changes. EMG testing can help distinguish between weakness due to muscle disease from weakness due to nerve problems. Nerve conduction study is usually done during the same visit and is a test to see how fast electrical signals move through a nerve.
MRI (Magnetic Resonance Imaging)
MRI is being used more frequently for dermatomyositis and can show changes suggesting muscle inflammation. Physicians may also use MRI to choose the best muscle for biopsy.
Muscle Biopsy
The role of a muscle biopsy in diagnosing DM is diminishing as we learn more about myositis antibodies and utilize newly released diagnostic criteria. When certain antibodies or a characteristic skin rash is present, a muscle biopsy may not be necessary.
When a muscle biopsy is necessary, a doctor will remove a small piece of muscle tissue, either via a needle biopsy or an open surgical biopsy, and send it to a lab for testing.
Your doctor will choose the weakest muscle, careful to avoid the site of any recent EMG, for biopsy. An MRI can be helpful in locating the best muscle to biopsy.
Skin Biopsy with skin exam
Biopsying the skin can be helpful in making a diagnosis of dermatomyositis. It is vital to find an experienced dermatologist as DM looks identical to Lupus on biopsy and a skin exam can help differentiate the two.
Other Testing
The above tests are not an exhaustive list your physician may use. Other testing will depend on your symptoms and coexisting illnesses. Some examples are below.
Cancer Screening
Since there is an increased risk and potential association of cancer with dermatomyositis, your doctor may perform several cancer screenings at diagnosis, and for years following, including those that are age and gender appropriate. Certain autoantibodies can help predict a risk of associated malignancy. These are undergoing more research.
Barium Swallow Test
If you have trouble swallowing, a barium swallow test may be ordered. This is a test often used to determine the cause of painful swallowing, difficulty with swallowing, abdominal pain, bloodstained vomit, or unexplained weight loss. Barium sulfate is a metallic compound that shows up on X-rays and is used to help see abnormalities in the esophagus and stomach.
CT Scan (computed tomography) and Chest X-ray
When lung involvement is suspected, a chest X-ray and CT scan of the lungs can help identify lung disease associated with myositis such as Interstitial Lung Disease (ILD).
Pulmonary Function Tests (PFT’s)
When the lungs are involved, your physician may order PFTs, a group of tests that measure how well your lungs work. This includes how well you are able to breathe and how effective your lungs are able to bring oxygen to the rest of your body.
Challenges of diagnosing Dermatomyositis
Diagnosing dermatomyositis may be a long and difficult process for several reasons.
Dermatomyositis is a rare disease. Rare diseases are inherently more difficult to diagnose. Do you know the saying, “When you hear hoofbeats, look for horses, not zebras?” This is something doctors are taught and in many cases works well. The “horses” are the most common illnesses and the “zebras” refer to the rare diseases, like DM.
Each patient with DM presents differently, so a clear pattern or set of symptoms is not necessarily visible to make a diagnosis.
The diagnosis can be delayed when characteristic findings are not present such as typical skin findings, proximal muscle weakness, elevated muscle enzymes such as creatine kinase (CK or CPK) and aldolase, myopathic findings on electromyography (EMG), and typical muscle/skin biopsy findings for dermatomyositis.
Dermatomyositis can mimic other diseases such as muscular dystrophies of late-onset, as well as adult-onset nemaline myopathy, proximal myotonic myopathies, systemic lupus erythematosus, pityriasis rubra pilaris, lichen planus, and polymorphous light eruption.
Other involvement with Dermatomyositis
Dermatomyositis may affect other organ systems, cause other illnesses, or place you at a higher risk of these developing.
- Raynaud’s phenomenon. This condition causes your fingers, toes, cheeks, nose and ears to turn pale when exposed to cold temperatures or stress.
- Other connective tissue diseases – Other conditions, such as lupus, rheumatoid arthritis, scleroderma and Sjogren’s syndrome, can occur with dermatomyositis (overlap syndromes).
- Cardiovascular complications – Dermatomyositis can cause heart muscle inflammation (myocarditis). In others who have dermatomyositis, heart arrhythmias and congestive heart failure may develop.
- Interstitial Lung Disease (ILD) – Interstitial lung disease refers to a group of disorders that cause scarring (fibrosis) of lung tissue, making the lungs stiff and inelastic.
Dermatomyositis is not polymyositis with skin involvement. PM and DM are very different diseases.
Dermatomyositis in images
Treating Dermatomyositis
The goals of treatment for dermatomyositis are to eliminate or reduce skin and muscle inflammation, restore muscle performance, reduce morbidity, and improve a patient’s quality of life.
There is one FDA-approved therapy for dermatomyositis, Octoagam 10% (IVIG), aside from oral, topical and IV steroids, which are not recommended for long-term use.
Finding a combination of medications is often necessary for successful results.
Sun Avoidance and protective measures
Sun avoidance, ample use of high SPF sunscreen, UVA and physical blockers are recommended. UV protected apparel, large brim hats, and sunglasses are also very helpful.
Corticosteroids
The initial treatment is typically corticosteroids such as prednisone or prednisolone and may be dosed by the patient’s weight at 1 mg per kg. Corticosteroids address inflammation and simultaneously help suppress the overactive immune system. Intravenous (IV) steroids may also be used.
Steroids have many side effects including weight gain and redistribution of body fat to the face, neck, and abdomen; elevated blood sugars, mood swings, thinning of the skin, cataracts, and osteoporosis.
Additional drugs to suppress the immune system are frequently added to the steroids, sometimes at the beginning of treatment and other times once the determination has been made that steroids have shown to be effective.
Since steroids, especially in high doses and over prolonged periods, are known to have many adverse side effects and may cause added health issues, the introduction of steroid-sparing medications should be considered.
Note: Corticosteroids should not be confused with anabolic steroids, used by some weightlifters and athletes, to enhance performance.
Immunosuppressive Drugs
Steroid-sparing agents, such as immunosuppressive drugs and Disease-Modifying Antirheumatic Drugs (DMARDs), have an added benefit as they often reduce or eliminate the need for steroids while also improving the symptoms of DM. However, these medications are not without their own risks.
Some commonly used immunosuppressive drugs include azathioprine (Imuran), mycophenolate mofetil (Cellcept), and Tacrolimus (Prograf). Cyclosporine (Neoral, Sandimmune) may also be used in difficult to treat cases.
Methotrexate (Rheumatrex) is commonly used and is available in pill form and as an injectable. For those with lung involvement, discuss the serious risks of using methotrexate.
Cytotoxic Drugs
Cytotoxic medications are a class of immunosuppressives that were originally developed and are still used, to treat certain types of cancer.
Cyclophosphamide (Cytoxan) is one of these medications used. It is available in a pill form and can be given intravenously (IV). This has been used to treat refractory cases of dermatomyositis.
Other Treatments
Antimalarial agents
Hydroxychloroquine (Plaquenil) is one of the commonly used drugs in this class and is used to treat the skin symptoms of DM. Others used may include chloroquine and quinacrine.
Immunoglobulin Therapy (IVIg, SubQ Ig)
Immunoglobulin comes from antibodies extracted from the plasma from thousands of blood donors. IVIg is the intravenous (IV) method.
SubQ Ig is also available, can be approved for some, is infused quicker under the skin, and eliminates the need for continuous home nursing.
Octagam® 10%
On July 20, the US Food and Drug Administration (FDA) granted approval to Octagam® 10% for the treatment of adult dermatomyositis. This is the first and only intravenous immunoglobulin (IVIg) approved for dermatomyositis.
Rituximab (Rituxan)
Rituximab belongs to a class of drugs called monoclonal antibodies. It is given intravenously (IV).
Acthar Gel
Acthar Gel, a corticotropin, is delivered either subcutaneously or via intramuscular injection, injected beneath the skin or into the muscle. It is a naturally-occurring hormone produced by the pituitary gland and has several potential mechanisms as to how it may benefit patients with DM. Acthar causes the release of cortisol from a patient’s adrenal glands, thus mimicking the effects of taking corticosteroids. Acthar also interacts with a number of receptors throughout the immune system and may reduce immune overactivity responsible for causing DM.
Plasmapheresis
Plasmapheresis (plasma exchange) is a process in which the fluid part of the blood, called plasma, is removed from blood cells by a device known as a cell separator. This process, in theory, removes antibodies that may cause DM. This treatment is not being used as much as it once was many years ago.
Living with Dermatomyositis
Day-to-day management of dermatomyositis can take many forms. Adapting to a “new normal” can be challenging and require many lifestyle changes.
Exercise Program
It was once thought exercise was dangerous for myositis patients and caused added muscle damage. This has now been proven false through research.
We now know there are massive benefits to having an approved exercise program, the sooner the better. This may start with your doctor, physical therapy, or a rehabilitation center. Movement/Exercise plans that are supervised by your medical and healthcare team are most effective so you do not injure yourself.
We have created an entire program around movement/exercise, and you are invited to join us!
Myositis Support Gets Moving on Clubhouse
Myositis Support Gets Moving is a safe space in our members-only Club on Clubhouse. In this program, we each create our own individualized movement plan and plan for proper protein intake in order to maintain and build muscle. This is not an exercise class, and you cannot fail in this group. We are here to provide ideas, motivation, encouragement, and to share successes and barriers so we can work together to keep moving, in whatever ways we can. If you are living with myositis or a care partner, join us here on Clubhouse.
Before starting any type of exercise plan, talk to your doctor first.
Diet and Nutrition
Eating a well-balanced diet high in protein may be beneficial for those with dermatomyositis, and is for your overall health.
Corticosteroids have many side effects including weight gain and redistribution of body fat to the face, neck, and abdomen, elevated blood sugars, and osteoporosis, so you may need to make adjustments in your diet for these conditions.
Ask your doctor about nutrition and a referral to a dietician or nutritionist.
Join us for Support
You are NOT alone. When living with dermatomyositis, having a good support system in place is extremely helpful.
Dermatomyositis is a chronic illness and some people in your life may not understand the disabling aspects of the symptoms, treatments, and stress involved in managing this complex, sometimes invisible illness. We understand because we are living with myositis, too.
Depression and anxiety can also be difficult aspects of this disease which may be exacerbated by the use of steroids.
We offer several online support options for patients, family members, caregivers, and friends of those living with DM. Having an emotional outlet is helpful, and our groups are educational, resourceful, and we even try to add some fun group activities to help members connect.
MSU provides a free, monthly online Zoom support session for those with dermatomyositis. This is a chance to meet others face-to-face, discuss challenges, share tips, and just talk to others who completely understand. View our Events page for upcoming support sessions.
Have you been diagnosed with dermatomyositis?
Get the support you deserve. Join the Myositis Support Community.
Safe, private myositis community for patients and caregivers.
Dermatomyositis Prognosis
The prognosis of dermatomyositis depends on many varying factors including patient response to treatment, the age of onset, the severity of disease and its manifestations, the presence of pulmonary or cardiac involvement, and if there is an associated malignancy.
Some dermatomyositis patients respond very well to treatment, while others do not respond at all. Finding the right treatment, or combination of treatments can take months to years.
Long-term steroid use may be a major source of morbidity.
Dermatomyositis In Focus
What does Dermatomyositis look like?
Dermatomyositis patients may require the use of assistive devices for mobility such as a cane, walker, or wheelchair, either for short period like during flares or for long-term muscle weakness and damage.
When the lungs are involved, some may wear oxygen.
DM patients may also wear long-sleeved shirts, hats, and gloves, even during the hottest months, to protect themselves as best as possible from the sun.
Some may look perfectly healthy on the outside, but on the inside, they are very sick and struggling on many levels.
Research and Clinical Trials
Research helps us better understand diseases and can lead to advances in diagnosis and treatment. As there are currently no approved treatments for DM, research is important, as are patients participating in clinical trials. There are several ongoing and upcoming clinical trials for skin-predominant dermatomyositis.
We have partnered with Antidote to help make your clinical trial match easier.
Simply Put
“Simply Put” is a service of Myositis Support and Understanding, to provide overviews of Myositis-related medical and scientific information in understandable language.
MSU volunteers, who have no medical background, read and analyze often-complicated medical information and present it in more simplified terms so that readers have a starting point for further investigation and consultation with healthcare providers. The information provided is not meant to be medical advice of any type.
Some images courtesy of The Muscular Dystrophy Association.