Sporadic Inclusion Body Myositis (sIBM)
Sporadic inclusion body myositis (sIBM) is one of a group of rare muscle diseases called inflammatory myopathies, and is a progressive muscle disease characterized by muscle inflammation, weakness, and atrophy (muscle wasting). Inclusion body myositis (IBM) is the most common aquired myopathy in those age 50 and older. The symptoms and rate of progression vary heavily from person to person.
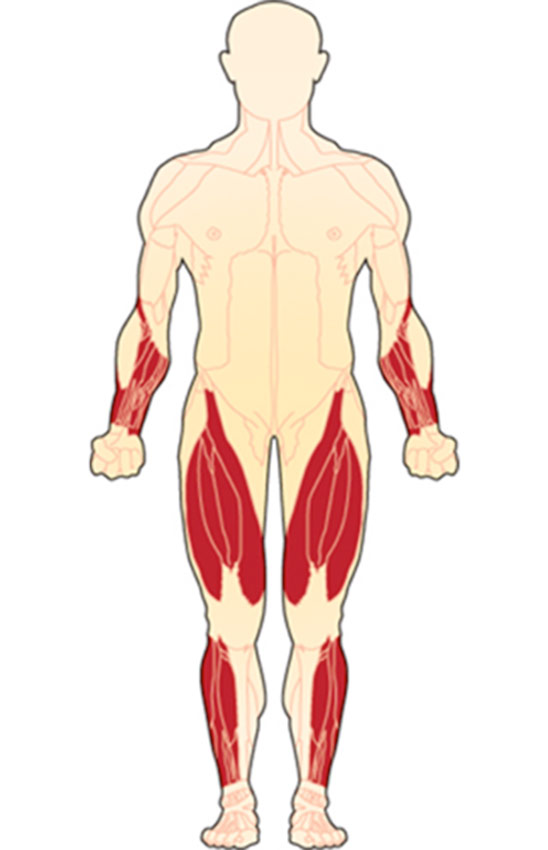
Muscle weakness tends to be asymmetric (greater on one side), involving the distal muscles, those furthest from the body’s core. Proximal muscles (closest to the core) may also be involved. IBM typically affects the muscles of the hands, fingers, arms and legs, particularly the thigh muscles (quadriceps), and muscles in the lower legs that move the feet.
Patients may have trouble pinching, buttoning, and holding items. Neck muscle weakness can cause the head to drop. Leg muscle weakness can cause difficulty rising from a chair, walking up stairs, and cause falls. “Foot drop,” caused by ankle muscle weakness, can lead to frequent falls. Some patients may also experience mild facial weakness.
Some Signs & Symptoms of sIBM
Complications/Progression of sIBM
Who is affected by Inclusion Body Myositis?
- IBM is the most common acquired muscle disorder in people over age 50.
- Symptoms of IBM may start in the 30’s and 40’s.
- IBM affects men somewhat more than women.
- Estimates indicate roughly 30,000 people are affected in the U.S. and major European countries combined.
NEW IndeeLift HFL-400-FTS
Designed because IndeeLift was contacted by several patients living with inclusion body myositis who needed a lift to raise them to a full standing position, we are announcing our partnership with Indeelift to provide a discount to those who need it most, you. And, for each machine sold in our community, IndeeLift will donate $200 for Myositis Medical and Patient-Centered Research and Development, with a commitment of up to $5M!
Learn more about the new IndeeLift and the program, and find helpful videos and details on how to add your name to the list to purchase.

Muscle Weakness and IBM
sIBM typically affects the distal muscles (those furthest from the body’s core). The weakness is asymmetric and is not uncommon for only one leg or one arm to be affected. Along with muscle weakness, muscle degeneration also occurs.
Many report initial weakness in the wrists, hands, and fingers, and the muscles at the front of the thigh (quadriceps). The muscles that lift the front of the foot may also be affected early on causing “foot drop” and a tendency to trip.
Muscle weakness in the fingers can affect the ability to grip objects and patients may have difficulty with things such as buttoning, pinching, and holding items like a pen.
In rare cases, muscle weakness in the neck can cause the head to drop and rest on the chest.
Due to the muscles involved, patients may also have trouble walking up stairs and rising from a sitting position.
Tools: Inclusion Body Myositis – Functional Rating Scale (IBM-FRS)
View detailed information about using the IBM-FRS at Cure IBM
LiftSeat, Powered toilet lifts
Inclusion Body Myositis patients may require many different assistive devices along the way to help live their day-to-day lives.
A powered toilet lift, such as LiftSeat, is an excellent option. Mention MSU to get $100 off any and all accessories.
More about LiftSeat for Myositis | LiftSeat for Myositis whitepaper
Inclusion Body Myositis Education Videos
Diagnosing Inclusion Body Myositis
Making a diagnosis of sIBM can often take many years. sIBM is typically a very slowly progressing and complex disease. Age of onset and disease progression can affect obtaining a proper diagnosis.
When symptoms first start, patients and physicians may dismiss the gradual onset of muscle weakness as “getting older” or part of aging.
sIBM may appear much like amyotrophic lateral sclerosis (ALS) as it affects middle-aged and older people and often affects the swallowing muscles early on.
sIBM may also appear much like polymyositis at first, in that both are inflammatory muscle diseases that involve skeletal muscle weakness of the arms and legs. A muscle biopsy can distinguish these two apart but findings can depend on the progression of the disease at the time of biopsy.
On muscle biopsy, a lack of “rimmed vacuoles” does not necessarily rule out sIBM. The symptoms, patient history, physical exam, blood tests, and other diagnostic tests will also assist in a diagnosis.
What type of doctor do I see?
sIBM is diagnosed and managed by either a rheumatologist or neurologist in combination with your primary care physician (PCP).
Neurologists, specifically neuromuscular specialists, will likely have more experience with sIBM. Consultation with other specialists may be required depending on symptoms and coexisting illnesses.
Exercise is important for sporadic inclusion body myositis patients and is the only prescribed therapy at this time. Therefore, you may also see a physical therapist, occupational therapist, and, if you have trouble swallowing (dysphagia), you may also see a speech-language pathologist.
Clinical and Physical Exam
A complete medical and family history is important in helping to diagnose a rare and complex disease such as sIBM. We suggest writing a detailed medical and family history that you can share with your medical team and that can be used for all future appointments.
The physical exam is very important and will likely include muscle testing.
Tips Finding a Myositis Specialist
Blood Testing
Your doctor may order various blood tests when suspecting sIBM. These are helpful in making a diagnosis and to help rule out other disorders and may include: autoimmune and inflammatory markers, myositis-specific and myositis-associated antibodies, and other antibodies. Additional blood tests may include:
- Creatine Kinase (CK or CPK) (muscle enzymes)
- Aldolase
- ALT and AST
- LDH (Lactate dehydrogenase)
- Sed Rate (also called ESR or Erythrocyte sedimentation rate)
- ANA (Antinuclear Antibodies panel)
- Anti-NT5C1A antibodies (found in some with sIBM)
EMG and Nerve Conduction Study (NCS)
An EMG (Electromyography) is a test that checks the health of the muscles and the nerves that control the muscles.
EMG testing can help distinguish between weakness due to muscle disease from weakness due to nerve problems. Nerve conduction study is usually done during the same visit and is a test to see how fast electrical signals move through a nerve. An EMG can rule out nerve disorders such as motor neuron disease (ALS) and peripheral neuropathy.
MRI (Magnetic Resonance Imaging)
MRI is being used more frequently for IBM and can show changes suggesting muscle inflammation and edema (swelling), muscle wasting, and fatty infiltration of muscles. Physicians may also use MRI to choose the best muscle for biopsy.
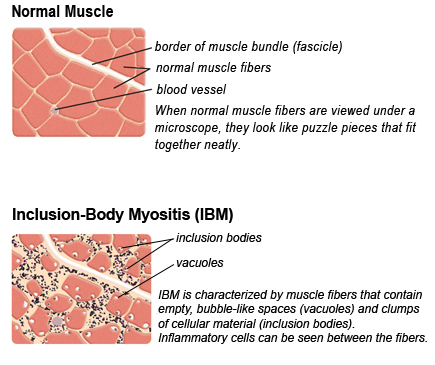
Muscle Biopsy
The muscle biopsy has long been considered the gold standard for a diagnosis of sIBM. A doctor will remove a small piece of muscle tissue, either via a needle biopsy or an open surgical biopsy, and send it to a lab for testing.
Your doctor will choose the weakest muscle, careful to avoid the site of any recent EMG, for biopsy. MRI can be helpful in locating the best muscle to biopsy.
Other Testing
The above tests are not an exhaustive list your physician may use. Other testing will depend upon your symptoms and coexisting illnesses.
Barium Swallow Test
If swallowing muscles are involved, a barium swallow test may be used. This test can be used to determine the cause of painful swallowing, difficulty with swallowing, abdominal pain, bloodstained vomit, or unexplained weight loss. Barium sulfate is a metallic compound that shows up on X-rays and is used to help see abnormalities in the esophagus and stomach.
Challenges of diagnosing sIBM
Diagnosing sIBM is often a difficult and years-long process for several reasons.
Sporadic inclusion body myositis is a rare disease. Rare diseases are inherently more difficult to diagnose. Have you heard the saying, “When you hear hoofbeats, look for horses, not zebras?” This is something doctors are taught and in many cases works well. The “horses” are the most common illnesses and the “zebras” refer to the rare diseases, like sIBM.
Each patient with sIBM presents differently, so a clear pattern or set of symptoms is not necessarily visible to make a diagnosis.
The diagnosis can be delayed when characteristic findings are not present such as typical muscle biopsy, MRI, and EMG findings.
sIBM symptoms can mimic other diseases such as muscular dystrophies of late-onset, polymyositis (PM), and motor neuron disease (ALS).
sIBM and Dysphagia
Dysphagia, weakness of the muscles involved in swallowing, can be a significant problem and contributing source of major complications such as choking and aspiration that can lead to dangerous pneumonias.
Dysphagia has been reported to affect 50 to 70% of IBM patients.
Sporadic Inclusion Body Myositis, in photos
IBM Muscle Biopsy
Muscle biopsy comparison of normal muscle tissue versus muscle tissues affected with Inclusion Body Myositis. Inclusion Body Myositis is named for the clumps of discarded cellular material — the “bodies” — that collect in the muscle tissues.
Image courtesy of The Muscular Dystrophy Association

Muscle Wasting
The first muscles affected in inclusion body myositis are usually those of the wrists and fingers, and the muscles at the front of the thigh. The muscles that lift the front of the foot also may be affected. This image shows muscle wasting in the forearm into the hands and fingers.
Treating IBM
There are currently no approved medications to treat sIBM. There are other things those with sIBM can do that may help improve their lives and/or slow the progression of the disease.
Exercise and sIBM
It was once thought exercise for myositis patients caused muscle damage. Through research, this is no longer the case.
We now know there are massive benefits in having an approved exercise program. This may start with a doctors referral to physical therapy or a rehabilitation center. Exercise plans that are supervised by your medical and healthcare team are most effective so you do not injure yourself. Be sure to consult with your doctor prior to beginning or changing an exercise program.
Going hand-in-hand with physical therapy, occupational therapy is also beneficial for inclusion body myositis patients.
In occupational therapy, you learn new ways to do things that might now be difficult due to muscle weakness. The therapist will work with you on things such as tying your shoes, ways to move things around on a table, and other more specific tasks. They will also assist with arm strengthening and fine motor skills.
Fall Prevention
Frequent unexplained falls are often a reason people seek medical attention.
Fall prevention is an important factor in staying safe with inclusion body myositis.
- Use assistive devices for mobility (cane, walker, rollator, wheelchair)
- Remove clutter in walkways like rugs, children and pet toys, and other items that may get caught on your foot when walking.
- Using grab bars, shower seats, and transfers for bathing can help keep you safe.
- Use of orthotics may help prevent falls.
- Having an alert system can be comforting for loved ones and can assist patients in case of falls. Google Home and Amazon Alexa both have these features. Programs such as a life alert system can also be beneficial.
Emotional Support
Life with a challenging disease like sIBM can be lonely and can lead to isolation, depression, and anxiety.
Living with a chronic illness, some people in your life may not understand the challenging aspects of the symptoms or the stress involved in managing this complex, sometimes even invisible illness.
Having a good support system is essential for patients.
- Join Support Groups
- Talk to family members, friends, and neighbors about asking for help
- Try to focus on what you are able to do
MSU provides a free, monthly online video support session just for sIBM patients. This is an opportunity to meet others face-to-face, discuss challenges, share tips, and just talk to others who completely understand. View our Events page for upcoming support sessions.
sIBM and other diseases
sIBM is not typically associated with an increased prevalence of other diseases such as cancer or interstitial lung disease, like with some other forms of inflammatory myopathies.
However, autoimmune disorders such as Sjögren’s syndrome, thrombocytopenia, and sarcoidosis have been reported in up to 15% of patients with sIBM.
Life expectancy with sIBM is not thought to be affected.
Have you been diagnosed with sIBM?
Or, are you a caregiver for someone who has been?
Get the support you deserve. Join the Myositis Support Community.
Safe, private myositis community for patients and caregivers.
Inclusion Body Myositis Prognosis
The prognosis of inclusion body myositis depends on many varying factors including how quickly the disease progresses, the severity of disease and its manifestations, dysphagia leading to aspiration pneumonias, and other coexisting illnesses. Typically, IBM is not thought to affect lifespan.
Sporadic Inclusion Body Myositis In Focus
What does Inclusion Body Myositis look like?
At the beginning of the disease, patients may not have any outward appearing symptoms, however, frequent unexplained falls and a weak hand grip may be noticeable to some.
As sIBM progresses, patients will require the use of assistive devices for mobility such as a cane, walker, or rollator. Upon further progression, usually after many years, the use of a wheelchair or power chair will become necessary.
Research and Clinical Trials
Research helps us better understand diseases and can lead to advances in diagnosis and treatment. As there are currently no approved treatments for sporadic inclusion body myositis, research is important, as are patients participating in clinical trials.
We have partnered with Antidote to help make your clinical trial match easier.
Familial Inclusion Body Myositis
Familial inclusion body myositis is an extremely rare condition that has been reported in multiple members of several different families. The symptoms of familial-IBM resemble those of sporadic inclusion body myositis (sIBM) including a later age of onset and a similar pattern of muscle involvement, especially the involvement of the quadriceps muscle and the muscles of the fingers and hands.
The MSU Inclusion Body Myositis closed Facebook support group has members with familial inclusion body myositis.
Hereditary inclusion body myopathies
These are not inflammatory myopathies
We provide the information below to help direct those with the hereditary inclusion body myopathies to resources they can use. These are not a part of the inflammatory myopathies.
Inherited Inclusion Body Myopathies (hIBM) are a group of rare genetic disorders. hIBM causes progressive muscle wasting and weakness that begins in young adulthood and into the early twenties and thirties and can lead to very severe disability within 10 – 20 years. hIBM NOT one of the Idiopathic Inflammatory Myopathies as it has a known genetic cause.
hIBM lacks lymphocyte inflammation (inflammation) therefore it is a “myopathy” rather than “myositis.”
The hereditary inclusion body myopathies may be inherited as autosomal dominant or recessive traits and are caused by mutations of specific genes.
Inclusion body myopathy with early-onset Paget disease and frontotemporal dementia (IBMPFD) is a part of the inherited inclusion body myopathy family.
Research and Further Reading
Neuropathy in sporadic inclusion body myositis: A multi-modality neurophysiological study. Clinical Neurophysiology. Lee, J. H., Boland-Freitas, R., Liang, C., Howells, J., & Ng, K (2020)
Dysphagia in Patients with Sporadic Inclusion Body Myositis: Management Challenges
Authors: Nika Mohannak,1 Gemma Pattison,2 Kathryn Hird,1 Merrilee Needham 1,3,4
Published: 5 December 2019 Volume 2019:12 Pages 465—474
Inclusion Body Myositis, Neurol Clin. 2014 Aug; 32(3): 629–646.
Mazen M. Dimachkie, MD, Professor of Neurology, Director, Neurophysiology Division, Director, Neuromuscular Section and Richard J. Barohn, MD, Gertrude and Dewey Ziegler Professor, Chairman
Study of Arimoclomol in Inclusion Body Myositis (IBM), Orphazyme, Clinical Trial
Advances in early diagnosis, therapy of inclusion body myositis
Current Opinion in Rheumatology
Simply Put
“Simply Put” is a service of Myositis Support and Understanding, to provide overviews of Myositis-related medical and scientific information in understandable language.
MSU volunteers, who have no medical background, read and analyze often-complicated medical information and present it in more simplified terms so that readers have a starting point for further investigation and consultation with healthcare providers. The information provided is not meant to be medical advice of any type.