Sun Protection Tips for those with dermatomyositis
Our goal isn’t to scare you from going out into the sun, rather we want to share some practical tips you should be aware of and ways that you can take charge to protect yourself from the harmful UVA and UVB rays from the sun.
Sun Protection Tips for those with dermatomyositis
Sun exposure has been proven to initiate flares, cause skin cancer, and induce painful, itchy rashes and bumps. By preparing for your day in the sun, or even a drive in the car or sitting in your home, you can help protect yourself. It’s all about getting into a habit of self-care.
Sun protection should be a part of our routines year-round, but even more so as the sun intensifies. Many of us, who are on steroids, immune-suppressing or modulating drugs, are rendered highly sensitive to sun damage by those medications. Also, people with myositis, especially but not limited to those with skin involvement, such as those with dermatomyositis, have a higher risk of malignancies, so protecting our skin becomes a required aspect of our treatment plan.
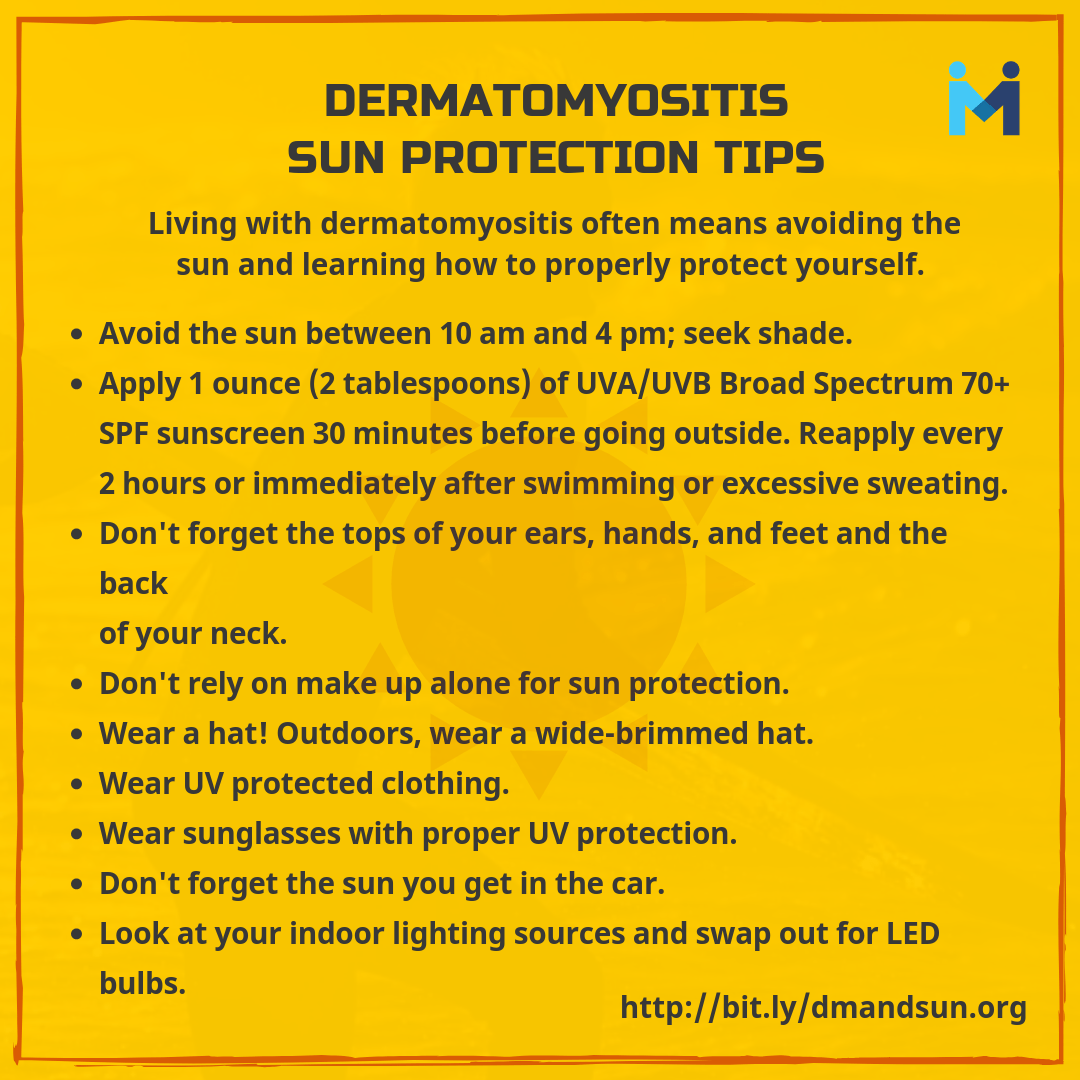
Follow a standard year-round protocol including:
- Seek the shade, especially between 10 AM and 4 PM.
- Do not burn!
- Avoid tanning and UV tanning beds.
- Cover up with clothing, including a broad-brimmed hat and UV-blocking sunglasses.
- Use a broad spectrum (UVA/UVB) sunscreen with an SPF of 30 or higher every day. For extended outdoor activity, use a water-resistant, broad-spectrum (UVA/UVB) sunscreen with an SPF of 30 or higher.
- Apply 1 ounce (2 tablespoons) of sunscreen to your entire body 30 minutes before going outside. Reapply every two hours or immediately after swimming or excessive sweating.
Some helpful sunscreen and sunblock tips
- Don’t forget the tops of your hands and feet, your face, back of your neck, and ears!
- Use at least a 30 SPF, 1 oz at a time ( a shot glass full), and reapply every 2 hours or so. For those with dermatomyositis and other photosensitivity, use a 70-100 SPF.
- Reapply after getting wet, toweling off, and sweating.
- For one day, you should expect to use ½ or ¼ of an 8oz bottle. You can buy more so apply liberally.
- Wear a wide-brimmed hat (3-inch brim is recommended)
- Avoid the sun between 10 AM-4 PM.
Sunscreen: The basics
There are so many sunscreens on the market that it is hard not to become confused about what is best for you.
What is sunscreen?
Simply put, sunscreen is a combination of ingredients that help prevent the sun’s ultraviolet (UV) radiation from reaching the skin. Two types of ultraviolet radiation, UVA and UVB, damage the skin, age it prematurely, and increase your risk of skin cancer, not to mention a Dermatomyositis or Lupus flare.
SPF 30 or higher is often recommended. SPF (sun protection factor) is a measure of the sunscreen’s ability to prevent UVB from damaging the skin. For those with dermatomyositis, clinically amyopathic dermatomyositis, and others with photosensitive conditions, using a 70 SPF or higher is recommended.
Generally, most dermatologists agree that it should be a UVA/UVB Broad Spectrum with an SPF of 30. Personal preference and experience may lead you to use higher levels. Some brands that have been recommended by dermatologists to us are EltaMD and Neutrogena Helioplex.
There are two types of protective lotions – chemical and physical.
Sunblock, the physical kind, contains both organic and non-organic ingredients that sit on top of the skin acting as a barrier between your skin and damaging UV rays by reflecting or scattering UVB light. Look for products with octyl methoxycinnamate, octyl salicylate and octocrylene.
Sunscreen, this is the chemical kind, penetrates the skin and absorbs the UVA rays before they are able to reach and damage your dermal layer. Zinc oxide and titanium dioxide are the active ingredients in deflecting harmful UV rays before they reach the protective outer epidermis layer of your skin.
Sunblocks are formulated to shield against UVB rays, while sunscreens protect against UVA. In order to fully protect your skin, choose a broad-spectrum protection formulated sunscreen that will protect against both UVA and UVB rays. Luckily these days, formulas often contain a mixture of both sunblock and sunscreen.
What is Broad Spectrum?
Broad-spectrum sunscreens protect the skin from both UVA and UVB rays and offer effective protection against both UVA (ultraviolet A) and UVB (ultraviolet B) rays.
What is SPF?
SPF stands for Sun Protection Factor. It is a rating for sunscreens or other cosmetic products containing sunscreen. Theoretically, the SPF number indicates how long you can stay in the sun before your skin reddens. SPF is only used to rate a sunscreen’s ability to protect against UVB rays.
Water resistant?
The terms “water-resistant” and “sweat-resistant” indicate whether the sunscreen remains effective for 40 minutes or 80 minutes when you are swimming or sweating. Since no sunscreen is fully “waterproof” or “sweatproof,” the FDA prohibits these terms.
Sunscreen Ingredients:
There are two main types of active sunscreen ingredients: chemical and physical.
Chemical ingredients such as avobenzone and benzophenone, work by absorbing UV, reducing its penetration into the skin, whereas physical ingredients such as titanium dioxide and zinc oxide stay on top of the skin and deflect UV rays. Many sunscreens available today combine chemical and physical ingredients.
Share with your Twitter friends!
Don’t forget your eyes!
Wear sunglasses with proper UV protection
It is easy to forget that our eyes, and the skin surrounding, can be severely damaged, over time, due to sun exposure, and even on cloudy days. By following some simple, daily steps, you can help yourself, and your eyes, from the potentials of vision loss and eye and eyelid cancers.
When you purchase sunglasses, check the tags, labels, or packaging to make sure the lenses have proper UV protection and the ability to absorb and block 99 to 100 percent of both UVA and UVB light. Ideally, they should also guard against HEV light.

- Be sure they fit to shield the eyes, eyelids, and surrounding areas. The more skin you cover, the better. Wraparound styles with a comfortable close fit and UV-protective side shields are ideal.
- Polarized lenses eliminate glare, especially when driving. They also increase comfort when you are out in the snow or on the water, where reflection greatly magnifies glare. Continuing glare can lead to fatigue, headaches, and even migraines.
- Also look to see if the glasses meet ANSI and/or ISO standards for traffic signal recognition, which means that the lenses permit good color recognition, especially for tasks such as discriminating red from green traffic signals.
- Sunglass lenses come in many shades; look for the lens color that provides you with the most comfortable vision.
- Contact lenses and prescription sunglasses both have the ability to have built-in sun protection.
If you detect symptoms of any problems with your eyes or eyelids, be sure to see a physician. Ophthalmologists have the greatest knowledge of eye conditions, while dermatologists are experts on the skin.
Seek Shade
While shade is a potentially valuable means of protection from the damaging effects of the sun’s ultraviolet (UV) rays, not all shade is equally protective. People can spend long hours in the shade while still receiving quite a lot of sun exposure and risking skin damage. This is because UVB rays, often considered the most harmful part of sunlight, can reach the skin indirectly.
Whenever you are outside, seek the shade, especially between 10 AM and 4 PM, when sunlight is the most intense and remember to use the tips above to properly protect yourself and your skin from the sun.
Sun you get in the car
Remember that even in the car you get sun exposure. And yes, even on cloudy days. Here are some tips to remember while in the car:
- Forgo the sunroof and convertible
- Keep sunscreen in the car
- Arms are at high risk so be sure to wear long sleeves with UV protected clothing
- Wear sunglasses
- Treat your car to window film
- Glass blocks only UVB effectively. Although car windshields are partially treated to filter out UVA, the side windows let in approximately 63% of the sun’s UVA radiation; rear windows are also unprotected, leaving back seat passengers exposed.

Sun you get under an umbrella
UV rays from the sun bounce off of water and sand. Therefore, even when sitting under an umbrella, you can get sun.
When using an umbrella, remember to utilize a host of other sun protection methods such as including a high SPF sunblock, UV protected clothing, wearing a wide-brimmed hat, and trying to avoid the sun during the most dangerous times of the day.
An umbrella is an excellent part of an overall sun protection routine!
Sun (UV) protected clothing
Clothing is our first line of defense against the sun’s harmful ultraviolet (UV) rays and protects us by absorbing or blocking much of this radiation. The more skin you cover, the better.
What is UPF?
UPF stands for Ultraviolet Protection Factor. It indicates what fraction of the sun’s ultraviolet rays can penetrate the fabric. A shirt with a UPF of 50, for example, allows just 1/50th of the sun’s UV radiation to reach the skin.
What Is the Difference Between UPF and SPF?
UPF is a rating generally used for clothing and other fabrics that protect you from the sun. It measures the amount of UVA and UVB radiation that penetrates the fabric and reaches the skin.
SPF stands for Sun Protection Factor. It is a rating for sunscreens or other cosmetic products containing sunscreen. Theoretically, the SPF number indicates how long you can stay in the sun before your skin reddens. SPF is only used to rate a sunscreen’s ability to protect against UVB rays.
Use the resources at the end of this page to find UV protected clothing, driving gloves, wide-brimmed hats, canopies, dress clothes, sportswear, bathing suits, umbrellas, and much, much more.
Medication photosensitivity
There are certain medications that we, as Myositis patients, take that can cause an increased reaction when we are exposed to the sun or even certain indoor lighting such as fluorescents.
Photosensitivity (or sun sensitivity) is inflammation of the skin induced by the combination of sunlight and certain medications or substances. This causes redness (erythema) of the skin and may look similar to sunburn. Both the photosensitizing medication or chemical and light source have to be present in order for a photosensitivity reaction to occur.
There are two categories: Phototoxic and Photoallergic reactions.
Phototoxic reactions
In a phototoxic reaction, the drug may become activated by exposure to sunlight and cause damage to the skin. The skin’s appearance resembles sunburn, and the process generally has a fast onset. UVA rays are most commonly associated with phototoxic reaction, however, UVB and visible light may also contribute. A rash from a phototoxic reaction generally clears up once you remain out of the sun, or the medication causing the reaction is stopped.
Symptoms of phototoxic reaction
Individuals with phototoxic reactions may initially complain of a burning and stinging sensation soon followed by redness of the sun-exposed areas of the body such as the forehead, nose, hands, arms, and lips. In severe cases, the sun protected areas of skin may be also be involved.
The range of skin damage may vary from mild redness to swelling to blister formation in more severe cases. The rash from this photosensitivity reaction usually resolves with peeling and sloughing off of the affected skin within several days.
Photoallergic reactions
In photoallergic reactions, the ultraviolet exposure changes the actual structure of the drug so that it is seen by the body’s immune system as an invader (antigen). The immune system initiates an allergic response (autoimmune) and causes inflammation of the skin in the sun-exposed areas. These reactions usually resemble eczema and are generally chronic, or long-lasting. Many drugs in this family are topical drugs.
This type of photosensitivity may recur after sun exposure even after the drug has cleared from the system and can sometimes spread to areas of the skin unexposed to the sun.
Symptoms of photoallergic reactions
Those with photoallergic reactions may initially complain of itching. This is then followed by redness and possibly swelling and eruption of the area involved. Since this is considered an allergic reaction, there may be no symptoms for many days when the drug is taken for the first time. Subsequent exposure to the drug and the sun may cause a more rapid response in 1-2 days.
Some common drugs that may lead to a photosensitivity reaction include:
- Antibiotics such as Cipro, Levaquin, doxycycline (those in the tetracycline family)
- DMARD’s/Chemo used to treat Myositis such as methotrexate
- Malaria medication used to treat Myositis such as hydroxychloroquine (Plaquenil)
- NSAIDs such as Naprosyn, Aleve, and ibuprofen
- Painkillers such as Celebrex
NOTE: This is a very short list of many medications that may cause a photosensitivity reaction.
Vitamin D Supplementation
If you are not able to spend time in the sun, a natural source of vitamin D, talk with your doctor about vitamin D supplements.
Your physician may, depending on your symptoms, order a vitamin D level as part of your myositis/autoimmune disease workup. Many autoimmune disease patients are vitamin D deficient.