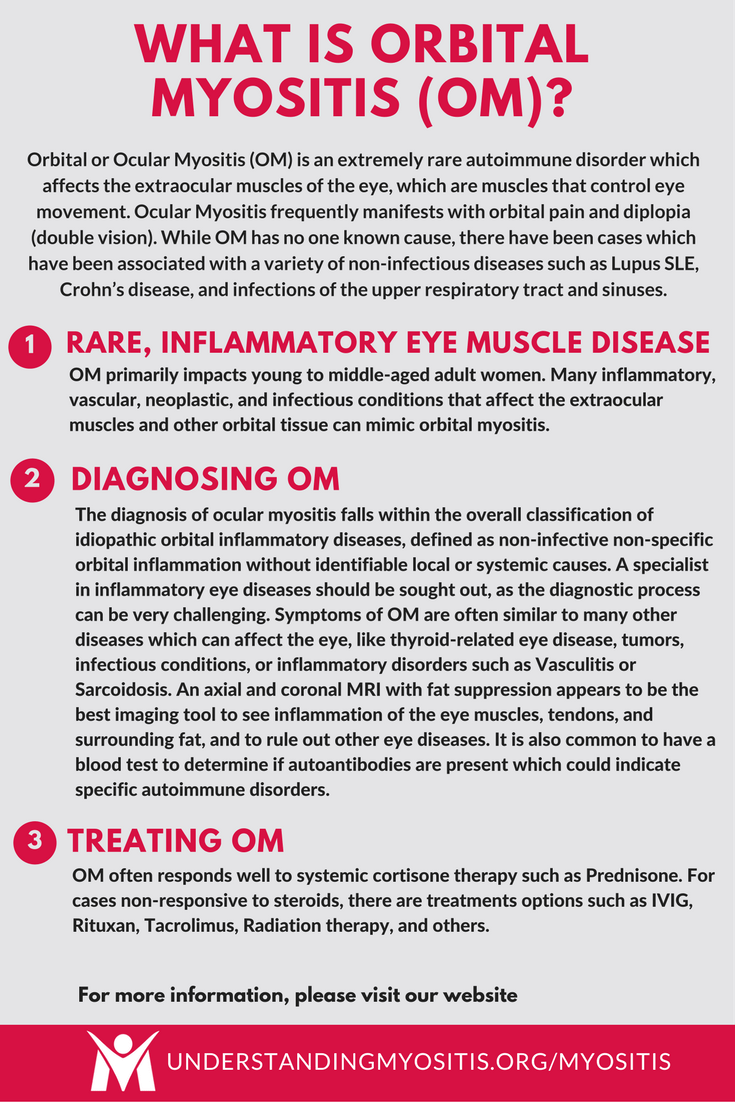
Orbital Myositis (OM)
Orbital or Ocular Myositis (OM) is an extremely rare autoimmune disorder which affects the extraocular muscles of the eye, which are muscles that control eye movement. Ocular Myositis frequently manifests with orbital pain and diplopia (double vision).
While OM has no one known cause, there have been cases which have been associated with a variety of non-infectious diseases such as Lupus SLE, Crohn’s disease, and infections of the upper respiratory tract and sinus.
Possible infectious causes for Orbital Myositis have been reported and may include Herpes Zoster, Lyme disease, and Cysticercosis, a rare parasitic infection.
OM primarily impacts young to middle-aged adult women.
Signs of Orbital Myositis
Quick Tips
Many inflammatory, vascular, neoplastic, and infectious conditions that affect the extraocular muscles and other orbital tissue can mimic orbital myositis.
The most important differential diagnoses include thyroid-related eye disease, other orbital inflammatory processes (unspecific idiopathic inflammation, vasculitis, and sarcoidosis), orbital cellulitis, and orbital tumors.
Diagnosing Orbital Myositis
 The diagnosis of ocular (ocular) myositis falls within the overall classification of idiopathic orbital inflammatory diseases, defined as non-infective non-specific orbital inflammation without identifiable local or systemic causes.
The diagnosis of ocular (ocular) myositis falls within the overall classification of idiopathic orbital inflammatory diseases, defined as non-infective non-specific orbital inflammation without identifiable local or systemic causes.
A specialist in inflammatory eye diseases should be sought out, as the diagnostic process can be very challenging. The cooperation of ophthalmologists and rheumatologists/immunologists will help to achieve a faster diagnosis and likely better treatment options.
The symptoms of OM are often similar to many other diseases which can affect the eye, such as thyroid-related eye disease, tumors, infectious conditions, or inflammatory disorders such as Vasculitis or Sarcoidosis.
An axial and coronal MRI with fat suppression appears to be the best imaging tool to see inflammation of the eye muscles, tendons, and surrounding fat, and to rule out other eye diseases.
It is also common to have a blood test to determine if autoantibodies are present which could indicate specific autoimmune disorders.
Treatment for Orbital Myositis
OM typically responds well to systemic cortisone therapy such as Prednisone.
Some cases which are non-responsive to steroid treatment, are chronic, or are recurrent may require other treatment options including:
Complications of Orbital Myositis
A prompt and proper diagnosis, with prompt and proper treatment, can dramatically improve symptoms in the majority of patients and may eliminate the disease altogether, although this is not a cure, as there is no cure at this time. However in some cases, especially in refractory ones, the disease can cause muscle fibrosis. A minority of patients may have recurrences.
The symptoms of OM are often similar to many other diseases which can affect the eye, such as thyroid-related eye disease, tumors, infectious conditions, or inflammatory disorders such as Vasculitis or Sarcoidosis.
An axial and coronal MRI with fat suppression appears to be the best imaging tool to see inflammation of the eye muscles, tendons, and surrounding fat, and to rule out other eye diseases.
It is also common to have a blood test to determine if autoantibodies are present which could indicate specific autoimmune disorders.
.
Get Support for OM
Orbital Myositis is really rare. Find others like you and get the support you deserve by joining our Myositis Support Community.
Join TodayOrbital Myositis Research and Articles
Myers (Provencher) LA, Vogelgesang SA, Kardon RH, Gordon LK, Shriver EM. Idiopathic Orbital Myositis: A Treatment Algorithm. EyeRounds.org. June 3, 2016. Available from http://EyeRounds.org/cases/234-Idiopathic-Orbital-Myositis.htm
Toshinobu Kubota (2011). Orbital Myositis. Idiopathic Inflammatory Myopathies – Recent Developments, Prof. Jan Tore Gran (Ed.), ISBN: 978-953-307-694-2, InTech, Available from http://www.intechopen.com/books/idiopathic-inflammatory-myopathies-recent-developments/orbital-myositis
Simply Put
“Simply Put” is a service of Myositis Support and Understanding, to provide overviews of Myositis-related medical and scientific information in understandable language.
MSU volunteers, who have no medical background, read and analyze often-complicated medical information and present it in more simplified terms so that readers have a starting point for further investigation and consultation with healthcare providers. The information provided is not meant to be medical advice of any type.