Polymyositis (PM)
Polymyositis is one of a group of rare muscle diseases called inflammatory myopathies, which are characterized by chronic muscle inflammation accompanied by muscle weakness.
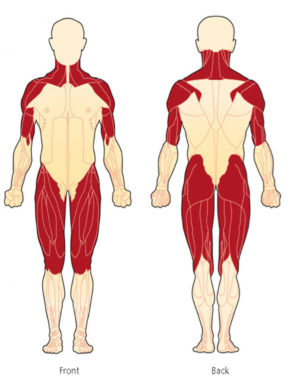
Muscle weakness can develop over a period of days, weeks, or months. This weakness often leads to difficulty climbing stairs, rising from a chair or from the floor, turning in bed, lifting, combing hair, or reaching over the head for something like an item on a shelf. Muscle weakness is typically symmetrical (same on both sides) and affects the proximal muscles (muscles closest to the body’s core) such as the hips, thighs, upper arms, shoulders, and neck.
Muscle pain (myalgia) and joint pain, with or without true arthritis and joint inflammation, can also be a part of polymyositis.
PM is a chronic, incurable disease.
Symptoms of Polymyositis
Symptoms vary from patient to patient
- Proximal muscle weakness (muscles closest to the body’s core), affecting upper arms, shoulders, thighs, hips, and neck
- Symmetrical muscle weakness (same on both sides of the body)
- Arthritis
- Muscle pain (myalgia)
- Difficulty swallowing (dysphagia)
- Fatigue (can be extreme and life-altering)
- Low-grade fever
- Labored breathing (dyspnea)
- A hoarse or changing voice when speaking (dysphonia)
- Difficulty maintaining enough air to finish a sentence
- Difficulty turning in bed, getting up from a seated position, and raising arms over the head
Other symptoms and complications
Potential complications, do not occur in all patients.
- Increased risk of falls
- Mechanic’s hands (roughening and cracking of the skin of the tips and sides of the fingers; the appearance of the hands of a mechanic)
- Aspiration pneumonia
- Interstitial lung disease (ILD)
- Raynaud’s phenomenon (fingers, toes, ears, feel numb and cool in response to cold temperatures or stress, often accompanied by changes in the color of the skin)
- Irregular heartbeat (arrhythmia)
- Increased risk of heart disease
- Inflammation in the heart (myocardium or inflammatory cardiomyopathy)
- Overlaps with other connective tissue diseases
- Increased risk of having certain types of cancer
Who is affected by Polymyositis?
Polymyositis is a rare disease. A rare disease in the U.S. is defined as a condition affecting fewer than 200,000 people.
Here is some additional information:
- PM affects twice as many women as men.
- PM, according to studies, is more common in African Americans, who are affected at five-times the rate of the Caucasian population in the U.S.
- PM typically occurs in adults over age 20, with many patients aged 45-60.
- It has been noted that a higher incidence of polymyositis is found in those in their mid-30’s-40’s and mid-50’s-60’s.
Other organ involvement and Polymyositis
Polymyositis is a systemic disease. This means PM can affect other organs of the body.
Lungs and Heart: Pulmonary disorders (interstitial lung disease) and less commonly, cardiac involvement (arrhythmia, pericarditis, myocarditis, congestive heart failure).
Antisynthetase Syndrome (ASS)
Approximately 90% of those diagnosed with Antisynthetase syndrome experience a form of myositis, either polymyositis or dermatomyositis. This complex syndrome also includes interstitial lung disease (ILD), Raynaud’s phenomenon, inflammatory polyarthritis, mechanic’s hands, and fever.
Mixed Connective Tissue Disease (MCTD)
Mixed connective tissue disease is a rare autoimmune disease considered an “overlap” of three diseases; Systemic Lupus Erythematosus, Scleroderma, and Polymyositis.
Overlap Syndrome
Overlap Syndrome means having more than one autoimmune disease at the same time. This can include many diseases such as Lupus, Dermatomyositis, Polymyositis, Scleroderma, Raynaud’s phenomenon, and Sjögren’s syndrome.
Cancer and Polymyositis
Cancer can be an underlying cause of polymyositis, but to a lesser extent than with Dermatomyositis. Cancer may precede the onset and if the cancer precipitated PM, removal or treatment of the cancer may result in the remission of polymyositis.
It is estimated that up to 10-15% of polymyositis in adults has also been linked to an increased likelihood of developing cancer post-diagnosis, particularly cancers of the cervix, lungs, pancreas, bladder, breasts, ovaries, and gastrointestinal tract, prostate as well as non-Hodgkin’s lymphoma. The risk of cancer appears to level off about three years after a diagnosis of PM. It is strongly suggested that appropriate cancer screenings be conducted upon diagnosis and in the years after a myositis diagnosis.
Pain and Polymyositis
Myalgia (muscle pain) is a reality for many polymyositis patients.
Studies and reports do not say how many experience pain, but an estimate based on information we received from an expert in the field, and who sees a large number of patients in a myositis center, reported 50% of patients in her practice experience pain.
Polymyositis: The evolution of this diagnosis in light of recent research
by Dr. Lisa Christopher-Stine
Diagnosing Polymyositis
Which doctors do I see?
Polymyositis is diagnosed and managed by either a rheumatologist or neurologist, with a neuromuscular specialist likely having the most experience, usually in coordination with a primary care physician (PCP). Consultation with other specialists may be required depending on your symptoms, other coexisting illnesses, and other organ involvement and may include a cardiologist, pulmonologist, oncologist, and pain management specialist.
Exercise is important for myositis patients. Therefore, you may also see a physical therapist, occupational therapist, and, if you have trouble swallowing (dysphagia), you may also see a speech-language pathologist.
Clinical and Physical Exam
A complete medical and family history are important in helping to diagnosis a rare and complex disease such as polymyositis. We suggest writing a detailed medical and family history that you can share with your medical team and that can be used for all future appointments.
Blood Testing
Your doctor will likely order various blood tests when suspecting polymyositis in order to measure autoimmune and inflammatory markers and to check for myositis-specific and myositis-associated antibodies, cancer markers (if suspected) and other antibodies. Some of these tests may include:
- Creatine Kinase (CK or CPK) (muscle enzymes)
- Aldolase
- ALT and AST
- LD (Lactate dehydrogenase)
- Sed Rate (also called ESR or Erythrocyte sedimentation rate)
- ANA (Antinuclear Antibodies panel)
EMG and Nerve Conduction Study (NCS)
An EMG (Electromyography) is a test that checks the health of the muscles and the nerves that control the muscles. With polymyositis, the EMG may show myopathic changes. EMG testing can help distinguish between weakness due to muscle disease from weakness due to nerve problems. Nerve conduction study is usually done during the same visit and is a test to see how fast electrical signals move through a nerve.
MRI (Magnetic Resonance Imaging)
MRI is being used more frequently for polymyositis and can show changes suggesting muscle inflammation. Physicians may also use MRI to choose the best muscle for biopsy.
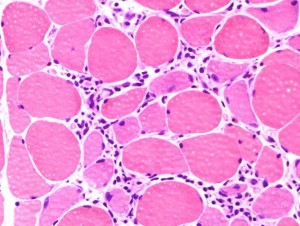
Muscle Biopsy
The muscle biopsy has long been considered a gold standard for a diagnosis of polymyositis. A doctor will remove a small piece of muscle tissue, either via a needle biopsy or an open surgical biopsy, and send it to a lab for testing.
Your doctor will choose the weakest muscle, careful to avoid the site of any recent EMG, for biopsy. An MRI can be helpful in locating the best muscle to biopsy.
Other Testing
The above tests are not an exhaustive list your physician may use. Other testing will depend upon your symptoms and coexisting illnesses. Some examples are below.
Cancer Screening
Since there is an increased risk and a potential association of cancer with polymyositis, your doctor may perform several cancer screenings, including those that are age and gender appropriate.
Barium Swallow Test
If you have trouble swallowing, a barium swallow test may be ordered. This is a test often used to determine the cause of painful swallowing, difficulty with swallowing, abdominal pain, bloodstained vomit, or unexplained weight loss. Barium sulfate is a metallic compound that shows up on X-rays and is used to help see abnormalities in the esophagus and stomach.
CT Scan (computed tomography) and Chest X-ray
When lung involvement is suspected, a chest X-ray and CT scan of the lungs can help identify lung disease associated with myositis such as Interstitial Lung Disease (ILD).
Pulmonary Function Tests (PFT’s)
When the lungs are involved, your physician may order PFTs, a group of tests that measure how well your lungs work. This includes how well you are able to breathe and how effective your lungs are able to bring oxygen to the rest of your body.
Challenges of diagnosing Polymyositis
Diagnosing polymyositis can be a long and difficult process for several reasons.
Polymyositis is a rare disease. Rare diseases are usually more difficult to diagnose. The saying, “When you hear hoofbeats, look for horses, not zebras” is something doctors are taught and in many cases works well. The “horses” are the most common illnesses and the “zebras” refer to the rare diseases, like PM.
Each patient with PM presents differently, so a clear pattern or set of symptoms is not necessarily visible to make a diagnosis.
The diagnosis can be delayed when characteristic findings are not present such as proximal muscle weakness, elevated muscle enzymes such as creatine kinase (CK or CPK) and aldolase, myopathic findings on electromyography (EMG), and typical muscle biopsy findings for PM.
Polymyositis can mimic other diseases such as adult-onset muscular dystrophies. There are also reports of patients first being diagnosed with polymyositis only later to find they have inclusion body myositis or a non-inflammatory myopathy.
Polymyositis in photos
Treating Polymyositis
The goals of treatment for polymyositis are to eliminate or reduce inflammation, restore muscle performance, reduce morbidity, and improve a patient’s quality of life.
There are no approved therapies for polymyositis, aside from steroids, which are not recommended for long-term use.
Finding a combination of medications is often necessary for successful results.
Corticosteroids
The initial treatment is typically corticosteroids such as prednisone or prednisolone and may be dosed by the patient’s weight at 1 mg per kg. Corticosteroids address inflammation and simultaneously help suppress the overactive immune system. Intravenous (IV) steroids may also be used.
Steroids have many side effects including weight gain and redistribution of body fat to the face, neck, and abdomen; elevated blood sugars, mood swings, thinning of the skin, cataracts, and osteoporosis.
Additional drugs to suppress the immune system are frequently added to the steroids, sometimes at the beginning of treatment and other times once the determination has been made that steroids have shown to be effective.
Since steroids, especially in high doses and over prolonged periods, are known to have many adverse side effects and may cause many other health issues, the introduction of steroid-sparing medications should be considered.
Note: Corticosteroids should not be confused with anabolic steroids, used by some weightlifters and athletes, to enhance performance.
Immunosuppressive Drugs
Steroid-sparing agents, such as immunosuppressive drugs and Disease-Modifying Antirheumatic Drugs (DMARDs), have an added benefit as they often reduce or eliminate the need for steroids while also improving the symptoms of polymyositis. However, these medications are not without their own risks.
Some commonly used immunosuppressive drugs include azathioprine (Imuran), mycophenolate mofetil (Cellcept), and Tacrolimus (Prograf). Cyclosporine (Neoral, Sandimmune) may also be used in difficult to treat cases.
Methotrexate (Rheumatrex) is commonly used and is available in pill form and as an injectable. For those with lung involvement, discuss the risks of using methotrexate.
Cytotoxic Drugs
Cytotoxic medications are a class of immunosuppressives that were originally developed and are still used to treat certain types of cancer.
Cyclophosphamide (Cytoxan) is one of these medications used. It is available in a pill form and can be given intravenously (IV). This has been used to treat refractory cases of polymyositis.
Other Treatments
Immunoglobulin Therapy (IVIg, SubQ Ig)
Immunoglobulin comes from antibodies extracted from the plasma from thousands of blood donors. IVIg is the intravenous (IV) method. SubQ Ig is also available, and can be approved for some, and is infused quicker under the skin and eliminates the need for continuous home nursing.
Rituximab (Rituxan)
Rituximab belongs to a class of drugs called monoclonal antibodies. It is given intravenously (IV).
Acthar Gel
Acthar Gel, a corticotropin, is delivered either subcutaneously or via intramuscular injection, injected beneath the skin or into the muscle. It is a naturally-occurring hormone produced by the pituitary gland and has several potential mechanisms as to how it may benefit patients with PM. Acthar causes the release of cortisol from a patient’s adrenal glands, thus mimicking the effects of taking corticosteroids. Acthar also interacts with a number of receptors throughout the immune system and may reduce immune overactivity responsible for causing PM.
Plasmapheresis
Plasmapheresis (plasma exchange) is a process in which the fluid part of the blood, called plasma, is removed from blood cells by a device known as a cell separator. This process, in theory, removes antibodies that may cause polymyositis. This treatment is not being used as much as it once was many years ago.
See more information about the medications and other treatments by visiting our Treating Myositis page.
Living with Polymyositis
Day-to-day management of polymyositis can take many forms. Adapting to a “new normal” can be challenging and require many lifestyle changes.
Exercise Program
It was once thought exercise was not good for myositis patients and caused muscle damage. This has now been proven false through research.
We now know there are massive benefits in having an approved exercise program. This may start with a doctors referral to physical therapy or a rehabilitation center. Exercise plans that are supervised by your medical and healthcare team are most effective so you do not injure yourself.
Before starting any type of exercise plan, talk to your doctor first.
Diet and Nutrition
Eating a well-balanced diet high in protein may be beneficial for those with polymyositis, and is for your overall health.
Corticosteroids have many side effects including weight gain and redistribution of body fat to the face, neck, and abdomen, elevated blood sugars, and osteoporosis, so you may need to make adjustments in your diet for these conditions.
Ask your doctor about nutrition and a referral to a dietician or nutritionist.
Support
When living with polymyositis, having a good support system in place is extremely helpful.
Polymyositis is a chronic illness and some people in your life may not understand the disabling aspects of the symptoms, treatments, and stress involved in managing this complex, sometimes even invisible illness.
We offer several online support options for patients, family members, caregivers, and friends of those living with polymyositis. Having an emotional outlet is helpful, and our groups are also educational and resourceful. We, at times, try to add some fun activities aimed at helping reduce stress and get to know one another better.
Have you been diagnosed with Polymyositis?
Get the support you deserve. Join the Myositis Support Community.
Safe, private myositis community for patients and caregivers.
Polymyositis Prognosis
The prognosis of polymyositis depends on many varying factors including patient response to treatment, the age of onset, the severity of disease and its manifestations, the presence of pulmonary or cardiac involvement, and if there is an associated malignancy.
Some polymyositis patients respond very well to treatment, while others do not respond at all. Finding the right treatment, or combination of treatments can take months-to-years.
Long-term steroid use may be a major source of morbidity.
Polymyositis In Focus
What does Polymyositis look like?
Polymyositis patients may require the use of devices to help with mobility such as a cane, walker, or wheelchair, either for short periods like during flares or for long-term muscle weakness and damage. When the lungs are involved, some may wear oxygen. Some may look perfectly healthy on the outside, but on the inside, they are very sick and struggling on many levels.
Research and Clinical Trials
Research helps us better understand diseases and can lead to advances in diagnosis and treatment. As there are currently no approved treatments for polymyositis, research is important, as are patients participating in clinical trials.
We have partnered with Antidote to help make your clinical trial match easier.
Simply Put
“Simply Put” is a service of Myositis Support and Understanding, to provide overviews of Myositis-related medical and scientific information in understandable language.
MSU volunteers, who have no medical background, read and analyze often-complicated medical information and present it in more simplified terms so that readers have a starting point for further investigation and consultation with healthcare providers. The information provided is not meant to be medical advice of any type and is in no way intended to replace professional medical care by a qualified specialist and should not be used as a basis for diagnosis or treatment.
Some images courtesy of The Muscular Dystrophy Association.